Have you ever experienced frequent heartburn or abdominal pain and wondered if it's a sign of something more serious? It's important to understand the difference between two common conditions: GERD (gastroesophageal reflux disease) and gallbladder issues. Although they can often present similar symptoms, knowing how to differentiate between the two is key in getting the right diagnosis and treatment.
Defining GERD and Gallbladder Issues
Let's start by understanding what GERD and gallbladder issues actually are.
GERD, also known as acid reflux, is a chronic condition where the stomach acid flows back into the esophagus, causing irritation and inflammation. This can lead to a range of uncomfortable symptoms, including heartburn, regurgitation, and chest pain.
The main culprit behind GERD is a weakened lower esophageal sphincter (LES), which fails to close properly, allowing stomach acid to escape. Other factors that can contribute to GERD include obesity, hiatal hernia, and certain lifestyle choices such as smoking or consuming certain foods and drinks.
GERD can have a significant impact on a person's quality of life. The constant discomfort and pain can make it difficult to enjoy meals or engage in daily activities. It can also lead to complications such as esophagitis, which is inflammation of the esophagus, and Barrett's esophagus, a condition that increases the risk of esophageal cancer.
What are Gallbladder Issues?
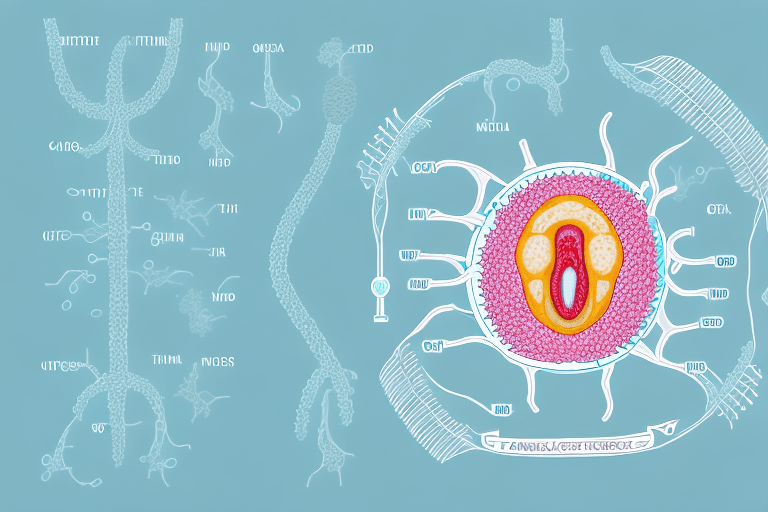
Gallbladder issues, on the other hand, refer to problems affecting the gallbladder, a small organ located below the liver. The gallbladder plays a critical role in storing bile, a substance produced by the liver that helps in digesting fats. When the gallbladder fails to function properly, various issues can arise.
Gallbladder issues can manifest as gallstones, inflammation (cholecystitis), or a blockage in the bile ducts. Gallstones are solid deposits that form in the gallbladder and can cause severe pain when they obstruct the flow of bile. Cholecystitis is the inflammation of the gallbladder, usually caused by gallstones. A blockage in the bile ducts can occur due to gallstones or other factors, leading to jaundice, a yellowing of the skin and eyes.
It is important to note that gallbladder issues can have different causes. Gallstones, for example, can form when there is an imbalance in the substances that make up bile, such as cholesterol or bilirubin. Other risk factors for gallbladder issues include obesity, a sedentary lifestyle, a high-fat diet, and certain medical conditions such as diabetes.
When someone experiences gallbladder issues, they may have to make significant changes to their diet and lifestyle. Fatty and greasy foods are often avoided to prevent triggering symptoms. In severe cases, surgical removal of the gallbladder, known as cholecystectomy, may be necessary to alleviate symptoms and prevent complications.
Symptoms of GERD and Gallbladder Issues
While GERD (gastroesophageal reflux disease) and gallbladder issues may share some symptoms, there are subtle differences that can help distinguish between the two. Understanding these differences is crucial for accurate diagnosis and appropriate treatment.
Common Symptoms of GERD
GERD is often characterized by a burning sensation in the chest, known as heartburn. This discomfort usually occurs after meals or when lying down and can be accompanied by an acidic taste in the mouth. The feeling of heartburn can be quite distressing, causing discomfort and pain.
In addition to heartburn, other telltale signs of GERD include regurgitation of food or sour liquid, difficulty swallowing, and a chronic cough. These symptoms can significantly impact an individual's quality of life, affecting their ability to eat, sleep, and engage in daily activities.
It's important to note that GERD symptoms may vary from person to person, and some individuals may experience only a few of these symptoms. This variability can make it challenging to diagnose GERD solely based on symptoms. Consulting with a healthcare professional is crucial for an accurate diagnosis.
Recognizing Gallbladder Issue Symptoms
Gallbladder problems can present with symptoms similar to GERD, making it important to pay close attention to the details. The primary symptom associated with gallbladder issues is intense abdominal pain, often occurring in the upper right quadrant. This pain can be sharp, cramp-like, or constant, and it may radiate to the back or right shoulder blade. The severity of the pain can vary from mild to excruciating, and it may worsen after eating fatty or greasy foods.
In addition to abdominal pain, nausea, vomiting, and indigestion are also commonly experienced with gallbladder problems. These symptoms can be quite uncomfortable and disruptive to daily life. If you notice yellowing of the skin or eyes (jaundice) or light-colored stools, it may indicate a more severe gallbladder condition that requires immediate medical attention.
It's worth noting that while GERD and gallbladder issues can share some symptoms, there are key differences that can help differentiate between the two. Consulting with a healthcare professional is essential for an accurate diagnosis and appropriate treatment plan.
Causes and Risk Factors
Understanding the underlying causes and risk factors for both GERD (Gastroesophageal Reflux Disease) and gallbladder issues can provide valuable insights into how these conditions develop and affect individuals.
What Causes GERD?
GERD can be caused by several factors, each playing a role in the development and exacerbation of the condition. One common cause is a weak lower esophageal sphincter (LES), which is the ring of muscle that separates the esophagus from the stomach. This weakness can be a result of genetics, where some individuals may have a naturally weaker LES. Additionally, certain medications, such as those used to treat asthma or high blood pressure, can relax the LES, making it more prone to allowing stomach acid to flow back into the esophagus.
Another contributing factor to GERD is a hiatal hernia, a condition where the upper part of the stomach protrudes into the chest through the diaphragm. This displacement of the stomach can disrupt the normal functioning of the LES, leading to acid reflux and heartburn.
Lifestyle choices also play a significant role in triggering or worsening GERD symptoms. Excessive alcohol intake can irritate the lining of the esophagus and increase stomach acid production. Smoking, on the other hand, weakens the LES and impairs the body's ability to clear acid from the esophagus. Additionally, consuming fatty or spicy foods can relax the LES and delay stomach emptying, making it easier for acid to reflux into the esophagus.
Risk Factors for Gallbladder Issues
Gallbladder issues, such as gallstones or inflammation (cholecystitis), tend to be more common in individuals who are overweight or obese. The excess weight puts additional pressure on the gallbladder, disrupting its normal functioning and increasing the likelihood of gallstone formation.
Hormonal changes during pregnancy also contribute to an increased risk of gallbladder issues. The surge in hormones, particularly estrogen, can affect the gallbladder's ability to empty properly, leading to the formation of gallstones. Furthermore, a sedentary lifestyle, characterized by a lack of physical activity, can impair gallbladder function and increase the risk of gallstone development.
Another significant risk factor for gallbladder issues is a high-fat diet. Consuming foods that are high in cholesterol and saturated fats can lead to an imbalance in bile composition, increasing the likelihood of gallstone formation. Additionally, individuals with a family history of gallstones are more prone to developing the condition themselves, suggesting a genetic predisposition.
It is worth noting that women are more susceptible to gallstone formation than men, especially during pregnancy or when using certain hormonal contraceptives. The hormonal changes and increased estrogen levels during these periods can contribute to the development of gallstones.
Diagnostic Procedures for GERD and Gallbladder Issues
Accurate diagnosis is crucial for determining the appropriate treatment plan for GERD or gallbladder issues. Different diagnostic procedures are utilized for each condition.
Diagnosing GERD
To diagnose GERD, your healthcare provider may start by conducting a thorough medical history and physical examination. This will involve asking you questions about your symptoms, such as heartburn, regurgitation, and difficulty swallowing. They will also inquire about your lifestyle habits, such as diet, smoking, and alcohol consumption, as these can contribute to GERD.
Further tests may be recommended to evaluate the extent of tissue damage and acid reflux. One common test is an upper gastrointestinal (GI) endoscopy, where a flexible tube with a camera is inserted through your mouth and into your esophagus and stomach. This allows the doctor to visually inspect the lining of your esophagus and stomach, looking for signs of inflammation, ulcers, or other abnormalities.
Another test that may be used is esophageal pH monitoring. This involves placing a small tube through your nose and into your esophagus to measure the amount of acid present over a 24-hour period. This test helps determine the frequency and severity of acid reflux episodes.
In some cases, lifestyle changes and response to medication can provide additional confirmation of a GERD diagnosis. If symptoms improve with dietary modifications, weight loss, and medication, it further supports the diagnosis of GERD.
How are Gallbladder Issues Identified?
When it comes to gallbladder issues, diagnostic procedures often include imaging tests, such as an ultrasound, CT scan, or MRI. These tests help identify any gallstones, inflammation, or abnormalities in the gallbladder or bile ducts.
An ultrasound is a common initial test used to visualize the gallbladder. It uses sound waves to create images of the gallbladder and surrounding structures. This can help identify the presence of gallstones, thickening of the gallbladder wall, or signs of inflammation.
In some cases, a CT scan or MRI may be ordered to provide more detailed images of the gallbladder and surrounding organs. These tests can help identify any structural abnormalities or complications, such as a blocked bile duct or infection.
In addition to imaging tests, blood tests may also be performed to check for elevated levels of liver enzymes, which can indicate gallbladder problems. These tests measure the levels of certain enzymes and bilirubin in the blood, providing further insight into the functioning of the gallbladder and liver.
Overall, a combination of medical history, physical examination, imaging tests, and blood tests is often used to diagnose gallbladder issues and determine the most appropriate course of treatment.
Treatment Options for GERD and Gallbladder Issues
The treatment approach for GERD and gallbladder issues differs based on the underlying cause and severity of symptoms. It is important to understand the various treatment methods available to effectively manage these conditions and improve quality of life.
Managing GERD: Medications and Lifestyle Changes
For mild cases of GERD, lifestyle modifications can often provide relief. These may include avoiding trigger foods that can exacerbate symptoms, such as spicy or fatty foods, caffeine, and alcohol. Additionally, maintaining a healthy weight through regular exercise and a balanced diet can help reduce the frequency and severity of GERD symptoms.
Elevating the head of the bed while sleeping can also help prevent acid reflux by keeping the stomach contents from flowing back into the esophagus. This can be achieved by using bed risers or placing a wedge pillow under the upper body.
Quitting smoking is another crucial step in managing GERD. Smoking weakens the lower esophageal sphincter (LES), the muscle responsible for preventing stomach acid from entering the esophagus. By quitting smoking, the LES can regain its strength and function properly, reducing the occurrence of acid reflux.
Over-the-counter antacids or acid reducers can help alleviate symptoms temporarily by neutralizing stomach acid or reducing its production. However, if symptoms persist or worsen, it is important to consult a healthcare provider for further evaluation and treatment.
In some cases, healthcare providers may prescribe stronger medications, such as proton pump inhibitors (PPIs) or H2 blockers, to reduce acid production or strengthen the LES. These medications can provide long-term relief and help heal any damage caused by GERD. However, it is important to follow the prescribed dosage and duration of treatment as advised by the healthcare provider.
In severe cases of GERD, surgery may be recommended to reinforce the lower esophageal sphincter or correct a hiatal hernia. These surgical interventions aim to improve the function of the LES and prevent the backflow of stomach acid into the esophagus. Surgical options may include fundoplication or LINX procedure, both of which provide long-term relief for GERD symptoms.
Treatment Methods for Gallbladder Issues
The most common treatment for gallstones is surgical removal of the gallbladder, known as cholecystectomy. This procedure is often performed using minimally invasive laparoscopic techniques, which involve making small incisions in the abdomen to insert a laparoscope and surgical instruments. Laparoscopic cholecystectomy offers several advantages over traditional open surgery, including shorter recovery time, reduced pain, and minimal scarring.
In certain cases, medication or other interventions may be prescribed to dissolve gallstones or alleviate symptoms. Ursodeoxycholic acid is a medication that can be used to dissolve cholesterol gallstones over time. However, this treatment method is only effective for certain types of gallstones and may take several months to show results.
If complications arise, such as an infection or blockage of the bile ducts, additional procedures like endoscopic retrograde cholangiopancreatography (ERCP) or percutaneous transhepatic cholangiography (PTC) may be required for treatment and management. ERCP involves using an endoscope to remove or break up gallstones, while PTC involves inserting a needle through the skin and into the liver to drain the bile ducts.
It is important to consult with a healthcare provider to determine the most appropriate treatment method for gallbladder issues based on individual circumstances and medical history.
In Conclusion
In summary, understanding the difference between GERD and gallbladder issues is crucial in determining the appropriate course of action for your symptoms. Although they can share similar symptoms, the underlying causes and treatment options for each condition vary. If you're experiencing persistent digestive discomfort, it's essential to seek medical advice to ensure an accurate diagnosis and tailored treatment plan.