GERD, or gastroesophageal reflux disease, is a chronic condition that affects the digestive system. It is characterized by the backflow of stomach acid into the esophagus, leading to a range of distressing symptoms. While most people are aware of the typical symptoms of GERD, such as heartburn and acid regurgitation, what they may not realize is that GERD can also cause back and chest pain. In this article, we will explore the connection between GERD and these types of pain, as well as discuss the diagnosis and treatment options for GERD.
Understanding GERD: A Brief Overview
Before delving into the link between GERD and back and chest pain, it is essential to have a basic understanding of GERD itself. GERD, short for gastroesophageal reflux disease, is a chronic digestive disorder characterized by the frequent backflow of stomach acid into the esophagus. This backflow can cause damage to the lining of the esophagus and lead to a range of unpleasant symptoms.
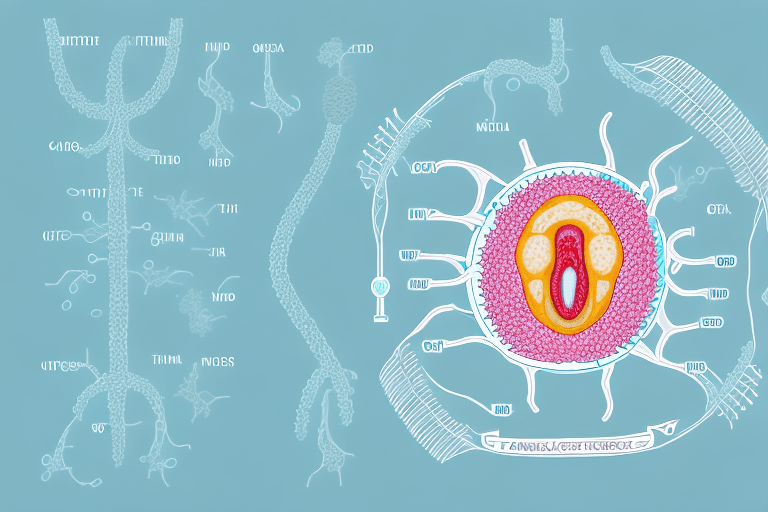
GERD occurs when the lower esophageal sphincter, a muscular ring that separates the esophagus from the stomach, malfunctions. This allows stomach acid to flow back into the esophagus, causing irritation and inflammation. The lower esophageal sphincter normally acts as a barrier, preventing the contents of the stomach from entering the esophagus. However, when it weakens or relaxes inappropriately, acid reflux occurs.
Common symptoms of GERD include heartburn, regurgitation of acid, difficulty swallowing, and a sour or bitter taste in the mouth. Heartburn is a burning sensation in the chest that often starts after eating and may worsen when lying down or bending over. Regurgitation is the sensation of acid backing up into the throat or mouth, sometimes accompanied by a sour or bitter taste. Difficulty swallowing, known as dysphagia, can occur when the esophagus becomes narrowed due to inflammation or scar tissue. This can make it challenging to swallow both solid and liquid foods.
GERD symptoms can vary in severity and frequency. Some individuals may experience occasional mild symptoms, while others may have more persistent and severe symptoms that significantly impact their quality of life. It is important to note that GERD is a chronic condition, meaning it requires ongoing management to control symptoms and prevent complications.
What is GERD?
GERD, short for gastroesophageal reflux disease, is a chronic digestive disorder characterized by the frequent backflow of stomach acid into the esophagus. This backflow can cause damage to the lining of the esophagus and lead to a range of unpleasant symptoms. While occasional acid reflux is common and not a cause for concern, GERD refers to a more severe and chronic form of acid reflux.
GERD can affect people of all ages, from infants to older adults. It is estimated that approximately 20% of the population in the United States experiences symptoms of GERD at least once a week. The prevalence of GERD has been increasing in recent years, likely due to various factors such as changes in diet, lifestyle, and obesity rates.
Common Symptoms of GERD
GERD can manifest in various ways, with symptoms ranging from mild to severe. The most common symptoms of GERD include heartburn, regurgitation of acid, difficulty swallowing, and a sour or bitter taste in the mouth. Heartburn is the hallmark symptom of GERD and is often described as a burning sensation in the chest that may radiate to the throat or even the back. It typically occurs after meals or when lying down.
Regurgitation of acid refers to the backflow of stomach contents into the throat or mouth. This can lead to a sour or bitter taste, as well as a feeling of a "lump" in the throat. Difficulty swallowing, or dysphagia, can occur when the esophagus becomes narrowed or constricted due to inflammation or scar tissue. This can make it challenging to swallow both solid and liquid foods, and may even cause choking or coughing during meals.
Other less common symptoms of GERD include chest pain, chronic cough, hoarseness, and dental erosion. Chest pain associated with GERD is often mistaken for a heart attack, as it can be intense and radiate to the arms, neck, or jaw. Chronic cough can be a result of acid irritating the throat and airways, while hoarseness may occur due to acid reflux affecting the vocal cords. Dental erosion, characterized by the wearing away of tooth enamel, can occur when acid repeatedly comes into contact with the teeth.
It is important to note that not everyone with GERD will experience all of these symptoms. Some individuals may only have one or two symptoms, while others may have a combination of several. If you suspect you may have GERD, it is important to consult with a healthcare professional for an accurate diagnosis and appropriate treatment plan.
The Connection Between GERD and Chest Pain
How GERD Triggers Chest Discomfort
One of the lesser-known symptoms of GERD is chest pain. The backflow of stomach acid into the esophagus can irritate the sensitive lining of the esophagus, leading to a burning sensation or discomfort in the chest. This pain is often mistaken for a heart-related issue, causing unnecessary worry and anxiety.
GERD-related chest pain typically occurs after a meal or when lying down, as these positions can exacerbate the backflow of stomach acid. It may also be accompanied by other symptoms such as heartburn or difficulty swallowing.
When stomach acid flows back into the esophagus, it can cause inflammation and damage to the esophageal lining. This can lead to the development of esophageal ulcers, which can further contribute to chest pain. The ulcers can cause a sharp, stabbing pain that is often felt behind the breastbone.
In addition to the physical discomfort, GERD-related chest pain can also have a significant impact on a person's quality of life. The pain can be disruptive and make it difficult to enjoy meals or engage in physical activities. It can also interfere with sleep, leading to fatigue and decreased productivity during the day.
Differentiating GERD Pain from Other Chest Pain
Although GERD-related chest pain may mimic the symptoms of a heart attack, there are several key differences to be aware of. Unlike heart-related chest pain, GERD pain primarily occurs after eating or while lying down. It is also not accompanied by shortness of breath, dizziness, or pain radiating down the left arm, which are common symptoms of a heart attack. However, if you are unsure about the origin of your chest pain, it is always important to seek medical attention promptly.
It is worth noting that GERD can also cause chest pain that is unrelated to the backflow of stomach acid. In some cases, the chest pain may be a result of the esophagus becoming hypersensitive to even small amounts of acid. This condition, known as functional heartburn, can cause chest pain that is similar to GERD-related pain but does not involve acid reflux.
Other potential causes of chest pain that should be considered include musculoskeletal issues, such as muscle strain or inflammation in the chest wall. Anxiety and panic attacks can also manifest as chest pain, making it important to consider the individual's mental health when evaluating the origin of the pain.
In conclusion, GERD-related chest pain can be a distressing symptom that is often mistaken for a heart-related issue. Understanding the triggers and characteristics of GERD pain can help differentiate it from other causes of chest discomfort. If you experience chest pain, it is always recommended to consult with a healthcare professional to determine the underlying cause and receive appropriate treatment.
Exploring the Link Between GERD and Back Pain
GERD and Upper Back Pain: Is There a Connection?
Alongside chest pain, GERD can also cause back pain, particularly in the upper back. This discomfort may be a result of the backflow of stomach acid irritating the nerves in the esophagus, which can radiate pain to the back. It is important to note that while GERD can cause back pain, not all cases of back pain are directly linked to GERD.
When stomach acid flows back into the esophagus, it can cause a burning sensation known as heartburn. However, this acid reflux can also affect the nerves in the surrounding area, leading to discomfort in the upper back. The connection between GERD and back pain is not fully understood, but it is believed that the irritation of the esophageal nerves can trigger pain signals that are interpreted as back pain.
GERD-induced back pain can vary in intensity and duration. Some individuals may experience a mild, dull ache, while others may suffer from a more intense, burning sensation. The pain may be constant or intermittent, depending on the severity of the acid reflux and the individual's sensitivity to pain.
Recognizing GERD-Induced Back Pain
GERD-induced back pain often occurs alongside other symptoms of GERD, such as heartburn or regurgitation of acid. These additional symptoms can help differentiate GERD-induced back pain from other musculoskeletal conditions that may cause similar symptoms.
It is important to pay attention to the timing and triggers of the back pain. If the pain is consistently experienced after meals or when lying down, it may be a sign of GERD-related discomfort. Additionally, if the back pain is relieved by antacids or other medications that reduce stomach acid, it further supports the possibility of GERD as the underlying cause.
However, it is crucial to consult a healthcare professional for an accurate diagnosis if you are experiencing persistent or severe back pain. They will be able to evaluate your symptoms, perform any necessary tests, and provide appropriate treatment options. Other potential causes of back pain, such as muscle strains, spinal issues, or other gastrointestinal conditions, need to be ruled out to ensure proper management of your symptoms.
In conclusion, while there is a link between GERD and back pain, it is essential to consider other factors and consult a healthcare professional for an accurate diagnosis. Understanding the connection between GERD and back pain can help individuals seek appropriate treatment and manage their symptoms effectively.
Diagnosis and Treatment of GERD
How is GERD Diagnosed?
Diagnosing GERD (gastroesophageal reflux disease) typically involves a combination of a detailed medical history, symptom evaluation, and diagnostic tests. Your healthcare provider will take the time to understand your symptoms and their frequency, as well as any factors that may aggravate or alleviate them. This comprehensive approach helps in accurately diagnosing GERD and ruling out other conditions that may present with similar symptoms.
One of the common diagnostic tests used for GERD is an upper endoscopy, also known as an esophagogastroduodenoscopy (EGD). During this procedure, a thin, flexible tube with a camera at the end is inserted through the mouth and into the esophagus, stomach, and small intestine. This allows the healthcare provider to visually inspect the lining of the esophagus and identify any signs of inflammation, irritation, or damage caused by acid reflux.
In addition to an upper endoscopy, pH monitoring may also be performed to assess the extent of acid reflux. This test involves placing a small catheter through the nose and into the esophagus to measure the pH levels over a 24-hour period. By monitoring the pH levels, healthcare providers can determine the frequency and duration of acid reflux episodes, which helps in guiding treatment decisions.
Imaging tests, such as a barium swallow or esophageal manometry, may also be used to evaluate the function and structure of the esophagus. A barium swallow involves swallowing a liquid containing barium, which coats the esophagus and allows for better visualization on X-rays. Esophageal manometry measures the pressure and movement of the esophagus to assess its function.
Effective Treatment Options for GERD
Treatment for GERD aims to reduce symptoms, heal esophageal inflammation, and prevent complications. The approach to treatment depends on the severity of the condition and the individual's response to initial interventions.
Lifestyle modifications play a crucial role in managing GERD. Avoiding trigger foods, such as spicy or fatty foods, caffeine, and alcohol, can help reduce the frequency and severity of acid reflux episodes. Maintaining a healthy weight is also important, as excess weight can put pressure on the stomach and increase the risk of acid reflux. Elevating the head of the bed by using a wedge pillow or raising the head of the bedframe can help prevent acid from flowing back into the esophagus while sleeping.
In mild cases of GERD, lifestyle modifications may provide sufficient relief. However, for more severe or persistent symptoms, medications may be necessary. Proton pump inhibitors (PPIs) are commonly prescribed to reduce the production of stomach acid and promote healing of the esophagus. These medications are available over-the-counter or by prescription, depending on the strength and duration of treatment required.
In some cases, surgical intervention may be recommended to manage GERD. Surgical options include fundoplication, a procedure that strengthens the lower esophageal sphincter to prevent acid reflux, and LINX device placement, which involves implanting a small magnetic ring around the esophagus to reinforce the sphincter. These surgical procedures are typically reserved for individuals who do not respond to lifestyle modifications or medications.
It is important to work closely with your healthcare provider to develop an individualized treatment plan for GERD. Regular follow-up appointments and open communication can help monitor the effectiveness of treatment and make any necessary adjustments to ensure optimal symptom control and overall well-being.
Lifestyle Changes to Manage GERD Symptoms
Dietary Adjustments to Reduce GERD Flare-ups
Modifying your diet can play a significant role in managing GERD symptoms. It is advisable to avoid foods and beverages that trigger acid reflux, such as spicy foods, citrus fruits, chocolate, and caffeine. Additionally, eating smaller, more frequent meals and avoiding lying down right after eating can help minimize symptoms.
The Role of Exercise in Managing GERD
Regular exercise can aid in managing GERD symptoms by promoting weight loss, reducing stress levels, and improving digestion. However, it is important to choose low-impact exercises and avoid intense physical activity immediately after a meal, as this can exacerbate symptoms. Consult with a healthcare professional or a qualified trainer to determine the most suitable exercise regimen for your specific needs.
When to Seek Medical Attention
Warning Signs and Symptoms
While GERD is a chronic condition, certain warning signs and symptoms should prompt immediate medical attention. If you experience chest pain that radiates to your arms, shoulders, or jaw, have difficulty swallowing, or are coughing up blood, it is crucial to seek medical intervention promptly. These symptoms may indicate a more serious complication of GERD or a different underlying condition that requires urgent attention.
The Importance of Timely Medical Intervention
Timely medical intervention is vital in managing GERD effectively and preventing complications. If left untreated, GERD can lead to esophageal ulcers, strictures, or Barrett's esophagus, a condition that increases the risk of developing esophageal cancer. By seeking proper medical care and adhering to the recommended treatment plan, individuals with GERD can find relief from their symptoms and improve their quality of life.
In conclusion, GERD can indeed cause back and chest pain due to the backflow of stomach acid into the esophagus. However, it is crucial to differentiate GERD-induced pain from other potentially serious conditions. Seeking a proper diagnosis and adopting appropriate lifestyle modifications and treatment options can help alleviate symptoms and manage GERD effectively. If you are experiencing persistent back or chest pain, it is always advisable to consult a healthcare professional for an accurate evaluation and guidance.