Antibiotics are a vital tool in the fight against bacterial infections, but they can have some unwanted side effects. One of the most common side effects is bloating. Bloating can be uncomfortable and even painful, and it can last for days or weeks after antibiotic treatment has ended.
In this guide, we will explore the relationship between antibiotics and bloating, factors that can influence bloating duration, and what YOU can do to reduce and even prevent future bloating caused by antibiotic overuse.
Understanding Bloating and Antibiotics
Before delving into the details of bloating after antibiotic use, it is essential to understand what bloating is and how antibiotics affect gut health. Antibiotics work by killing bacteria, both good and bad, in the body. This can disrupt the natural balance of bacteria in the gut, known as your gut microbiome, leading to bloating and other digestive issues.
What is Bloating?
Bloating is a common digestive problem that can be caused by various factors, including overeating, stress, and food intolerances. It is characterized by a feeling of fullness, discomfort, and tightness in the abdomen.
Bloating can be caused by excess gas in the digestive system, which can result from poor digestion, certain foods, or bacterial imbalances in the gut which is known as dysbiosis.
There are many possible causes of bloating, including eating foods you are intolerant to, overconsuming carbonated beverages, and eating highly processed foods. Certain medical conditions, such as irritable bowel syndrome (IBS) and inflammatory bowel disease (IBD) and medications like antibiotics can also cause bloating.
How Antibiotics Affect Gut Health
Antibiotics work by killing bacteria in the body, including beneficial bacteria in the gut. While antibiotics are essential for treating bacterial infections, they can also have unintended consequences for gut health.
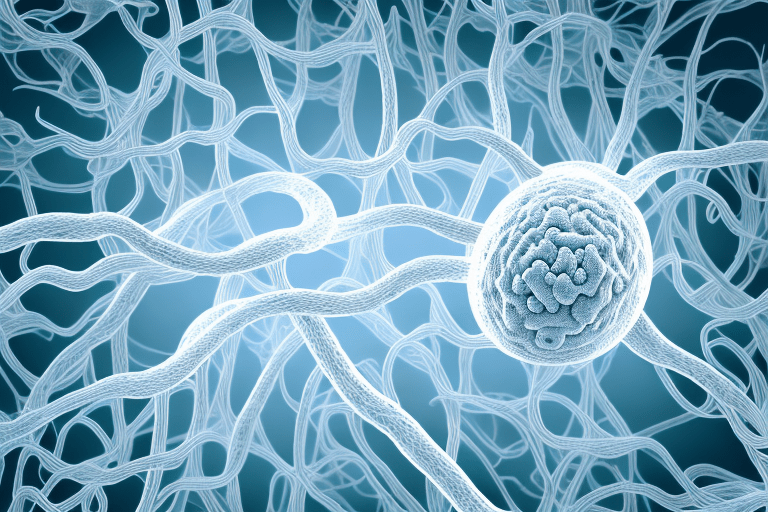
The gut microbiome, which is the collection of microorganisms that live in your gut, play a crucial role in digestion, immune function, and overall health. When antibiotics disrupt the natural balance of bacteria in the gut, it can lead to a range of digestive issues.
In addition to bloating, antibiotics can cause diarrhea, constipation, and abdominal pain. These symptoms can be mild or severe, depending on the type of antibiotic used, the dosage, and individual factors such as the health of your gut microbiome before antibiotics and pre-existing digestive issues.
In some cases, antibiotics can also lead to the development of antibiotic-resistant bacteria, like H pylori, which can be difficult to treat and pose a serious risk to public health. At GoodGut Nutrition, we prefer a herbal approach to kill H pylori instead of antibiotics as the first line of treatment.
Common Antibiotics Associated with Bloating
While most antibiotics can cause bloating as a side effect, some are more commonly associated with this symptom. These antibiotics include tetracycline, amoxicillin, and clindamycin.
It is important to note that not everyone who takes these antibiotics will experience bloating, and the severity and duration of symptoms can vary widely.
If you are prescribed one of these antibiotics and experience bloating, you may need to start to rebuild your gut microbiome using products like PolyPower, a unique blend of polyphenols that feed your gut bacteria.
In some cases, switching to a different antibiotic or adjusting the dosage may help alleviate symptoms. It is also important to take antibiotics only as prescribed and to finish the full course of treatment, even if symptoms improve.
Factors Influencing Bloating Duration After Antibiotics
The duration of bloating after antibiotic use can vary widely depending on several factors. Understanding these factors can help you prepare for and mitigate post-antibiotic bloating.
Type of Antibiotic
The type of antibiotic used can have an impact on the severity and duration of bloating after treatment. For example, broad-spectrum antibiotics such as ciprofloxacin and levofloxacin are associated with a higher risk of bloating and other digestive issues compared to narrow-spectrum antibiotics such as penicillin.
It is important to note that while broad-spectrum antibiotics may be necessary in certain situations, they should be used judiciously to avoid unnecessary disruption of the gut microbiome and potential digestive issues.
Dosage and Duration of Treatment
The dosage and duration of antibiotic treatment can also influence the severity and duration of bloating after treatment. Higher doses and longer treatment durations are associated with a higher risk of bloating and other digestive issues.
It is important to follow your doctor's instructions for dosage and duration of antibiotic treatment, and to avoid stopping treatment early even if you start to feel better. Stopping treatment early can increase the risk of antibiotic resistance and other complications.
Individual Gut Microbiome, Are You Protected?
Each person's gut microbiome is unique, and this can affect how their digestive system reacts to antibiotics. The "stronger" and more diverse your microbiome, the less likely you will have problems. Conversely, the weaker your microbiome diversity, the more likely you are to experience bloating.
There are several ways to support a healthy gut microbiome, including eating a diverse and balanced diet, avoiding unnecessary antibiotic use, and taking probiotics or other gut-friendly supplements like PolyPower, which contains select polyphenols which enrich and feed your microbial diversity, reducing bloating and discomfort.
Pre-existing Digestive Issues
If you already have pre-existing digestive issues such as irritable bowel syndrome (IBS), you may be more susceptible to bloating after antibiotic use. Talk to your doctor about ways to manage your symptoms and minimize post-antibiotic bloating.
There are several strategies that may be helpful for managing IBS symptoms, such as stress reduction techniques, dietary changes, and medication. Your doctor can help you determine the best approach for your individual needs.
It is also important to note that while antibiotics can be an important tool for treating bacterial infections, they are not effective against viral infections such as the common cold or flu. Using antibiotics unnecessarily can contribute to antibiotic resistance and other complications, so it is important to use them only when necessary and as directed by your healthcare provider.
Tips for Reducing Bloating After Antibiotic Use
If you experience bloating after antibiotic treatment, there are several things you can do to reduce and manage your symptoms. Bloating is a common side effect of antibiotics as they can disrupt the natural balance of bacteria in the gut, leading to an overgrowth of harmful bacteria and yeast. This can cause gas to build up in the digestive system, leading to uncomfortable bloating and abdominal pain.
Probiotics and Gut Health
Probiotics are beneficial bacteria that can help restore the natural balance of bacteria in the gut. Eating foods rich in probiotics such as yogurt, kefir, and sauerkraut can help reduce bloating and other digestive issues after antibiotic use. Probiotics can also help boost the immune system and improve overall gut health. While probiotic supplements are available, it is important to talk to your doctor before starting any new supplements to ensure they are safe and effective for you.
Dietary Changes to Minimise Bloating
Changing your diet can also help reduce bloating after antibiotic use. Avoiding foods that can cause gas such as beans, broccoli, and cabbage can help alleviate bloating symptoms. You may also consider increasing your fiber intake to help regulate digestion. Fiber can help keep the digestive system moving smoothly and prevent constipation, which can contribute to bloating. A microbiome friendly diet and good sources of fiber include fruits, vegetables, whole grains, and legumes.
In addition to avoiding gas-causing foods, it is important to eat a balanced diet that includes plenty of nutrients to support overall health. This can include lean protein sources such as chicken, fish, and tofu, as well as healthy fats like avocado and olive oil.
Hydration and Exercise
Staying hydrated and engaging in regular exercise can also help reduce bloating. Drinking plenty of water can help flush out excess gas and waste, while exercise can help stimulate digestion and regulate bowel movements. Aim to drink at least eight glasses of water per day and engage in moderate exercise for at least 30 minutes most days of the week. This can include activities like walking, running, cycling, or swimming.
Over-the-Counter Remedies
Over-the-counter remedies such as simethicone can help alleviate bloating symptoms. These remedies work by breaking down gas bubbles in the digestive system, making them easier to pass. However, it is important to talk to your doctor before using any over-the-counter remedies to ensure they are safe and effective for you.
Bloating after antibiotic use is a common issue that can be managed with a combination of dietary changes, probiotics, prebiotics, hydration, exercise, and over-the-counter remedies. By taking steps to support gut health and overall wellness, you can reduce your symptoms and feel more comfortable after antibiotic treatment.
When to Seek Medical Attention
In most cases, bloating after antibiotic use is a temporary and manageable side effect. However, in some cases, bloating can indicate a more serious underlying condition.
Persistent or Severe Bloating
If your bloating symptoms persist for more than a few weeks or are severe, you should talk to your doctor. This could indicate an underlying condition such as a gastrointestinal infection or inflammatory bowel disease.
Additional Symptoms to Watch For
In addition to bloating, you should watch for other digestive symptoms such as diarrhea, constipation, and abdominal pain. These could indicate a more serious underlying condition and should be evaluated by a medical professional.
Preventing Future Bloating Issues
To minimize the risk of bloating after antibiotic use in the future, talk to your doctor about strategies to protect your gut health such as boosting gut bacteria with PolyPower. This may include taking probiotics or avoiding antibiotics when possible. Maintaining a healthy diet and exercise routine can also help promote overall gut health.
Final Thoughts
Bloating is a common and often uncomfortable side effect of antibiotics. By understanding the relationship between antibiotics and bloating and taking steps to mitigate your symptoms, you can reduce the impact of bloating on your overall health. If you experience persistent or severe bloating after antibiotic use, talk to your doctor to rule out any underlying conditions that may require treatment.